Articles
- Page Path
- HOME > J Educ Eval Health Prof > Volume 17; 2020 > Article
-
Educational/faculty development material
Guidelines for the management of extravasation -
Jung Tae Kim1*
 , Jeong Yun Park2
, Jeong Yun Park2 , Hyun Jung Lee1
, Hyun Jung Lee1 , Young Ju Cheon1
, Young Ju Cheon1
-
DOI: https://doi.org/10.3352/jeehp.2020.17.21
Published online: August 10, 2020
1Department of Pharmacy, Kyung Hee University Hospital at Gangdong, Seoul, Korea
2Department of Clinical Nursing, University of Ulsan, Seoul, Korea
- *Corresponding email: jtkim@khnmc.or.kr
© 2020, Korea Health Personnel Licensing Examination Institute
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- The purpose of these practice guidelines is to offer and share strategies for preventing extravasation and measures for handling drugs known to cause tissue necrosis, which may occur even with the most skilled experts at intravenous (IV) injection. Herein, general knowledge about extravasation is first described, including its definition, incidence, risk factors, diagnosis, differential diagnosis, and extravasation injuries. Management of extravasation includes nursing intervention and thermal application. At the first sign of extravasation, nursing intervention with following steps is recommended: stop administration of IV fluids immediately, disconnect the IV tube from the cannula, aspirate any remaining drug from the cannula, administer drug-specific antidote, and notify the physician. Local thermal treatments are used to decrease the site reaction and absorption of the infiltrate. Local cooling (ice packs) aids in vasoconstriction, theoretically limiting the drug dispersion. Although clear benefit has not been demonstrated with thermal applications, it remains a standard supportive care. The recommended application schedule for both warm and cold applications is 15 to 20 minutes, every 4 hours, for 24 to 48 hours. For prevention of extravasation, health professionals should be familiar with the extravasation management standard guidelines. They should regularly check the extravasation kit, assess patients’ sensory changes, tingling or burning, and always pay attention to patients’ words. The medical team’s continuous education on extravasation is essential. With the practical use of these guidelines, it is expected to reduce the occurrence rate of extravasation and contribute to patient care improvement.
- Extravasation refers to the leakage of injected drugs from blood vessels causing damage to the surrounding tissues. Common symptoms and signs of extravasation include pain, stinging or burning sensations, and edema around the intravenous (IV) injection site. In severe cases, extravasation may cause tissue dysfunction or physical defects, resulting in a delay of attempted treatment, patients’ distrust, and numerous other issues. To prevent extravasation, a clinical specialist should perform the venipuncture or injection, who with relevant skills and management ability understands the properties of the injected drug. The primary purpose of these guidelines is to minimize the side-effects of IV injection, by suggesting proper and prompt emergency measures for extravasation and the appropriate treatments corresponding to the properties of the injected drug. The second purpose is to raise the medical team’s awareness of extravasation in order to prevent extravasation with careful injection, recover patient trust, and increase patient satisfaction. These guidelines consist of following topics: basic knowledge about extravasation, extravasation management, and extravasation prevention. Antidotes, special drug management, drugs with high osmolarity, and drugs with pH are provided as supplement files (Supplements 1–4). These contents are derived from authors’ experiences and the references [1-21]. It is anticipated that these guidelines would help health professionals to prevent extravasation during IV and central vein injection and to promote patient safety should extravasation occur in any case.
Introduction
- Definition
- Extravasation is the leakage of an injected drug out of the blood vessels, damaging the surrounding tissues. In terms of cancer therapy, extravasation refers to the inadvertent infiltration of chemotherapeutic drugs in the tissues surrounding the IV site.
- Extravasated drugs are classified according to their potential for causing damage as ‘vesicant,’ ‘irritant,’ and ‘nonvesicant.’ Vesicant drugs are also classified into 2 groups: DNA binding and non-DNA binding.
- Incidence
- The frequency of extravasation in adults is reported to be between 0.1% and 6%. Some data suggest that the incidence is decreasing probably due to improvements in the infusion procedure, early recognition of the drug leakage, and training in management techniques.
- Risk factors
- Risk factors can be classified under patient-related, procedure-related, and product or product-related factors.
- - Small and fragile veins in infants, children, or elderly patients
- - Vessels that may burst easily
- - Cancer patients with hardened and thickened vessels due to frequent venipuncture
- - Patients with vessels that move easily during venipuncture attempts
- - Patients with excised lymph nodes, limb amputation, or closed vena cava
- - Obesity in which peripheral venous access is more difficult
- - Patients who move around a lot
- - Untrained or inexperienced staff
- - Multiple attempts at cannulation
- - High flow pressure
- - Inadequate choice of equipment (peripheral catheter choice, size, or steel needle)
- - Inadequate dressings
- - Poor cannula fixation
- Diagnosis
- Patients must be informed to report any changes in sensation, signs, or symptoms during the IV administration of any chemotherapeutic drug and to alert the healthcare professionals to early signs of extravasation. Particular information must be given when a vesicant drug is administered. Extravasation must be suspected if any of the following specific signs or symptoms are presented (Table 1).
- - Possibly no initial symptoms of extravasation
- - Redness, pruritus, and edema around the injection site
- - Fluid injection rate slows down or stops
- - Blood backflow does not work well or there is leakage of medication around the needle
- - A complaint of discomfort or pain and occasional expression of searing pain or numbness
- - Initial physical symptoms usually appear immediately but also might appear several days or weeks later.
- - Often causes stinging pain
- - Edema around the port insertion or in the chest, or medication leakage around the catheter insertion
- - Redness in the chest, collarbone, or neck where a central venous catheter is inserted
- - No blood backflow
- - Symptoms may appear early or late.
- Differential diagnosis
- Spots or solid lines with blisters can be suddenly felt along the vessels injected with drugs. Pain, edema, and ulcer do not appear, and symptoms disappear within 30 to 90 minutes.
- Pain, tightening, and skin discoloration tend to worsen. Blood backflow works well, and edema or ulcer do not occur. Pain or tightening occurs along the vein, and it is caused mainly by drugs such as vinorelbine and dacarbazine. Hot fomentations can be applied to the dilated veins to mitigate the symptoms.
- Occurs due to contraction of the vessel wall and usually happens as soon as the fluid injection begins. For the most part, blood does not backflow. Discoloration and edema do not occur. Venous shock can occur when injecting very cold medication or when medication is injected at a rapid pace. Hot fomentations can dilate the veins and mitigate the symptoms.
- Extravasation injuries
- While the injury is usually minor and resolves spontaneously, some cases result in serious complications, including full-thickness skin loss and muscle and tendon necrosis requiring reconstructive surgery or even amputation, leading to longer hospital stays, increased morbidity, and increased costs.
- Narcotic analgesics may be required to reduce severe pain around widespread extensive necrosis.
- Patients may be unable to work for some time; quality of life must be compensated for if a patient’s occupation requires full physical mobility, and exposure of the disfigurement in public can cause a psychological impact.
- Depending on the situation, patients will bear the cost of hospitalization and medical expenses for cosmetic surgeries, and secondary medical problems might occur if the condition worsens.
- Treatment suspension wastes time and other problems can occur due to delayed treatment. If bone marrow function decreases, anticancer treatments may be delayed due to infection caused by leukopenia.
- The patient’s normal activities, such as at home, work, school, etc., may be disrupted until the patient is fully recovered.
- Therapists will always feel nervous during the medical team-patient communication because of guilt. Communication and trust between patients and nurses can be interfered due to extravasation.
Extravasation
Patient-related factors
Procedure-related factors
Product or product-related factors
In the case of peripheral IV catheter
In the case of central venous catheter
Flare reaction
Vessel irritation
Venous shock
Pain
Physical defects
Medical expense
Disease control
Time
Psychological impact on the nurse and the patient
- Nursing interventions
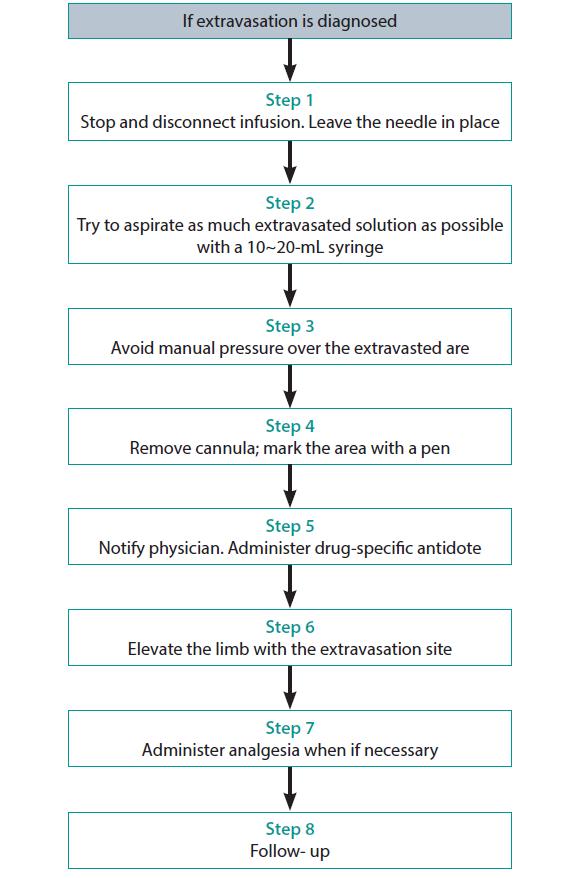
- At the first sign of extravasation, the following steps are recommended: (1) stop administration of IV fluids immediately, (2) disconnect the IV tube from the cannula, (3) aspirate any residual drug from the cannula, (4) administer a drug-specific antidote, and (5) notify the physician (Fig. 1).
- Elevation of the limb may aid in reabsorption of the infiltrate or extravasated vesicant by decreasing capillary hydrostatic pressure. Apply sterile dressing over the area of extravasation, regularly assess the extravasation site during every shift, and take medical photographs and consult the department of cosmetic surgery if necessary.
- Thermal application
- Local thermal treatments are used to decrease the site reaction and absorption of the infiltrate. Local cooling (ice packs) aids in vasoconstriction, theoretically limiting the drug dispersion. Cold application is recommended for extravasation of DNA-binding vesicants except for mechlorethamine (nitrogen mustard), contrast media, and hyperosmolar fluids. The use of local warming therapy (dry heat) is based on the theory that it enhances vasodilation, thus enhancing the dispersion of the vesicant agent and decreasing drug accumulation in the local tissue. The use of local warming is recommended for the extravasation of non–DNA-binding vesicants. Although clear benefit has not been demonstrated with thermal applications, it remains a standard supportive care, and the recommended application schedule for both warm and cold applications is 15 to 20 minutes, every 4 hours, for 24 to 48 hours.
- - It causes contraction of blood vessels, minimizing the spread of drugs to other tissues and reducing topical infections and pain.
- - Directions: apply cold fomentations for 15 to 20 minutes four to 6 times per day (for 1 day or more).
- - It dilates the blood vessels around the extravasation site, increases dispersion and absorption of the medicinal fluid by increasing the blood flow, and helps to quickly purge medicinal fluid that has leaked from the extravasation site.
- - Directions: apply hot fomentations for 20 to 30 minutes four to 6 times per day (for 1 day or more).
- Documentation
- Because errors associated with IV administration can result in fatal or life-threatening outcomes, administration of IV fluids and medications can be a high-risk, with adverse outcomes potentially leading to malpractice claims.
- An incident of extravasation must be correctly documented and reported. Documentation procedure may differ between treatment centers (documentation form); however, certain items are mandatory for patient safety and legal purposes: (1) patient name and number, (2) date and time of the extravasation, (3) name of the drug extravasated and the diluent used (if applicable), (4) signs and symptoms (also reported by the patient), (5) description of the IV access, (6) extravasation area (and the approximate amount of the drug extravasated), and (7) management steps with time and date.
- Photographic documentation can be helpful for follow-up procedures. The patient must be informed of the scope of the problem (Supplement 5).
Management of extravasation
Local cooling
Local warming
- General guidelines
- Most extravasations can be prevented with the systematic implementation of careful, standardized, and evidence-based administration techniques. The staff involved in the infusion and management of cytotoxic drugs must be trained to implement several preventive protocols for the minimization of the risk of extravasation. It is important to remember that the degree of damage is dependent on the type of the drug, the drug concentration, the localization of the extravasation, and the length of time for which the drug develops its potential for damage.
- - Be familiar with the extravasation management standard guidelines and prepare the extravasation kit.
- - Regularly check the extravasation kit and refill any used medications. Extravasation kit includes the following: 25G needle, 10-cc syringe, and 1-mL syringe; disinfection swabs, sterile gauze, and adhesive bandage; saline solution (1 ampule); sterile distilled water (1 ampule); dimethyl sulfoxide 99% solution; hyaluronidase 1,500 U/mL (refrigerated); hydrocortisone cream 1%; sodium thiosulfate 25% solution; and warm pack and an ice pack (frozen).
- - Assess patient’s sensory changes, tingling or burning, and always pay attention to the words of patients.
- Preventive strategies: peripheral venous access device extravasation
- - Do not insert the cannula in the joints because it is difficult to secure, and neural damage and tendon injury can be caused if extravasation occurs due to vesicant drugs.
- - Do not insert the cannula in the antecubital fossa area, where it is extremely difficult to detect extravasation.
- - Veins on the back of the hand can be used, and in some cases, observation is easier. But it must be done carefully because this area can suffer a more severe injury due to extravasation.
- - For observation, do not cover the cannula area with opaque gauze.
- - Secure the cannula during the administration of the drug.
- - Even if there is an existing IV route, secure a new route when administering vesicant drugs.
- - If in doubt, re-insert the cannula and administer the drug.
- - Watch for edema, inflammation, and pain around the cannula during administration.
- - Check for blood backflow before/during administration, and always rinse the catheter with a saline solution in between administrations.
- - Dilute stimulant drugs as much as possible and inject them at a proper rate.
- - Once the needle is removed, apply pressure to the puncture site for about five minutes and elevate the limb.
- Preventive strategies: central venous access device extravasation
- - Check for blood backflow before injection to ensure that the catheter is positioned in the vein.
- - Check if there is any local discomfort or swelling by running a saline solution through the catheter, and then inject the drug.
- - After the injection, make sure to run a saline solution through the catheter.
Prevention of extravasation
- Extravasation is a serious complication during patient care. Although drugs can be administered by methods (e.g., micro-patch, micro-injection) other than IV injection, extravasation cannot be totally avoided because there are drugs that can only be administered through IV or central vein injection. The guidelines described herein are based on the authors’ best practice for the management and prevention of the extravasation. However, no guidelines can be perfect, and they need to be regularly updated. It will be our pleasure if these guidelines are used in the training of health professionals to promote patients’ safety.
Conclusion
-
Authors’ contributions
Conceptualization: JTK, JYP, HJL, YJC. Data curation: JTK, JYP, HJL, YJC. Project administration: JTK, JYP, HJL, YJC. Visualization: JTK, JYP, HJL, YJC. Writing–original draft: JTK, JYP, HJL, YJC. Writing–review & editing: JTK, JYP, HJL, YJC.
-
Conflict of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Data availability
None.
Article information
Acknowledgments
Supplementary materials
-
Editors’ note: I found this booklet, guidelines for the management of extravasation on November 15, 2019, at the 2019 Fall Conference of the Korean Society for Clinical Pharmacology and Therapeutics. It is the brilliant info like a diamond that is useful for the training of the interns, nurses, and medical laboratory technicians who routinely work for the vascular injection. I remember the case of the complication of extravasation in my patient in 1985 when I was an intern. The patient should receive the skin graft for recovering her arm skin. If I understood the guidelines for extravasation management, it might be possible to prevent the necrosis of her arm skin. This guideline will enable health professions to manage the patients’ extravasation appropriately.
Article information
- 1. Drug information: Clinical Computerized Information System: vol. 113. Englewood (CO): Micromedex Inc; [date unknown]
- 2. BIT Druginfo website [Internet]. Seoul: BIT Druginfo; 2020 [cited 2020 Jul 10]. Available from: http://www.druginfo.co.kr
- 3. The National Extravasation Information Service website [Internet]. [place unknown]: The National Extravasation Information Service; 2020 [cited 2020 Jul 10]. Available from: http://www.extravasation.org.uk
- 4. Policy for the management of extravasation of intravenous drugs [Internet]. [place unknown]: [publisher unknown]; 2018 [cited 2020 Jul 10]. Available from: https://www.nwcscnsenate.uk/files/8114/7334/9859/Final_Extravasation_Policy_V5.0_June_18.pdf
- 5. Lacy C; American Pharmaceutical Association. Drug information handbook. 8th ed. Hudson (OH): Lexi-Comp Inc; 2000.
- 6. Barton-Burke M, Wilkes GM, Ingwersen KC, Bean CK, Berg D. Cancer chemotherapy: a nursing process approach. 2nd ed. Sudbury (MA): Jones and Bartlett Publishers; 1996.
- 7. Finley RS. Concepts in oncology therapeutics: a self-instructional course. Bethesda (MD): American Society of Hospital Pharmacists; 1991.
- 8. Hadaway L. Extravasation: Issues and Controversies. Proceedings of the Infusion Nurses Society Annual Meeting; 1997 May; Salt Lake City, USA. Norwood (MA): Infusion Nurses Society; 1997.
- 9. Nursing Department, Asan Medical Center. Nursing standard for intravenous injection of Asan Medical Center. Seoul: Asan Medical Center; 2007.
- 10. Yarbro CH, Wujcik D, Gobel BH. Cancer symptom management. 4th ed. Burlington (MA): Jones & Bartlett Learning; 2013.
- 11. Bragalone DL. Drug information handbook for oncology: a complete guide to combination chemotherapy regimens. 12th ed. Hudson (OH): Lexi-Comp Inc; 2014.
- 12. Reynolds PM, MacLaren R, Mueller SW, Fish DN, Kiser TH. Management of extravasation injuries: a focused evaluation of noncytotoxic medications. Pharmacotherapy 2014;34:617-632. https://doi.org/10.1002/phar.1396 ArticlePubMed
- 13. Common non-antineoplastic drugs that can act as vesicants or irritants [Internet]. Waltham (MA): UpToDate Inc; c2020 [cited 2020 Jul 10]. Available from: http://www.uptodate.com
- 14. University of Illinois College of Pharmacy. Drug Information Group [Internet]. Chicago (IL): University of Illinois College of Pharmac; c2020 [cited 2020 Jul 10]. Available from: http://www.uic.edu/pharmacy/centers/drug_information_center/faq/extravasation.php
- 15. Le A, Patel S. Extravasation of noncytotoxic drugs: a review of the literature. Ann Pharmacother 2014;48:870-886. https://doi.org/10.1177/1060028014527820 ArticlePubMed
- 16. Management of extravasation policy: version 01 [Internet]. NHS. Manchester: The Christie NHS Foundation Trust; 2014 [cited 2020 Jul 10]. Available from: https://manchestercancer.files.wordpress.com/2014/09/extravasation_sept20131.pdf
- 17. De Wit M, Ortner P, Lipp HP, Sehouli J, Untch M, Ruhnke M, Mayer-Steinacker R, Bokemeyer C, Jordan K. Management of cytotoxic extravasation: ASORS expert opinion for diagnosis, prevention and treatment. Onkologie 2013;36:127-135. https://doi.org/10.1159/000348524 ArticlePubMed
- 18. Perez Fidalgo JA, Garcia Fabregat L, Cervantes A, Margulies A, Vidall C, Roila F; ESMO Guidelines Working Group. Management of chemotherapy extravasation: ESMO--EONS clinical practice guidelines. Eur J Oncol Nurs 2012;16:528-534. https://doi.org/10.1016/j.ejon.2012.09.004 ArticlePubMed
- 19. Guideline for the management of extravasation of a cytotoxic agent or a monoclonal antibody used in the treatment of malignant disease: version 4.2. Worcester: Worcestershire Acute Hospitals NHS Trust; 2015.
- 20. Sauerland C, Engelking C, Wickham R, Corbi D. Vesicant extravasation part I: mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum 2006;33:1134-1141. https://doi.org/10.1188/06.ONF.1134-1141 ArticlePubMedPDF
- 21. Langer SW. Extravasation of chemotherapy. Curr Oncol Rep 2010;12(4):242-246. https://doi.org/10.1007/s11912-010-0110-7 ArticlePubMedPDF
References
Figure & Data
References
Citations

-
Exploring the multifaceted effects of
Ammi visnaga
: subchronic toxicity, antioxidant capacity, immunomodulatory, and anti-inflammatory activities
Martin Ndayambaje, Hicham Wahnou, Marieme Sow, Oumaima Chgari, Thierry Habyarimana, Mehdi Karkouri, Youness Limami, Abdallah Naya, Mounia Oudghiri
Journal of Toxicology and Environmental Health, Part A.2024; 87(4): 150. CrossRef - Extravasation and infiltration: under-recognised complications of intravenous therapy
Andrew Barton
British Journal of Nursing.2024; 33(7): S18. CrossRef - Safe and Informed Use of Gadolinium-Based Contrast Agent in Body Magnetic Resonance Imaging: Where We Were and Where We Are
Francesca Iacobellis, Marco Di Serafino, Camilla Russo, Roberto Ronza, Martina Caruso, Giuseppina Dell’Aversano Orabona, Costanza Camillo, Vittorio Sabatino, Dario Grimaldi, Chiara Rinaldo, Luigi Barbuto, Francesco Verde, Giuliana Giacobbe, Maria Laura Sc
Journal of Clinical Medicine.2024; 13(8): 2193. CrossRef - Nurses’ knowledge and experience related to short peripheral venous catheter extravasation
Selma Atay, Şengül Üzen Cura, Sevda Efil
The Journal of Vascular Access.2023; 24(4): 848. CrossRef - An updated narrative review on the management of the most common oncological and hematological emergencies
Ali Issani
Disease-a-Month.2023; 69(2): 101355. CrossRef - Peripheral venous extravasation injury
M.J. Billingham, R. Mittal
BJA Education.2023; 23(2): 42. CrossRef - Extravasation injuries in the intravenous therapy with drugs with properties vesicants and irritants in the veterinary medicine of small animals
Paolo Ruggero Errante
Journal of Dairy, Veterinary & Animal Research.2023; 12(1): 19. CrossRef - Sensing Technologies for Extravasation Detection: A Review
Ikue Hirata, Arianna Mazzotta, Pooyan Makvandi, Ilaria Cesini, Chiara Brioschi, Andrea Ferraris, Virgilio Mattoli
ACS Sensors.2023; 8(3): 1017. CrossRef - Skin Staining Following Intravenous Iron Extravasation in a Patient With Chronic Kidney Disease: A Case Report
Ruolin Shi, Judith G. Marin, Monica Beaulieu
Canadian Journal of Kidney Health and Disease.2023; 10: 205435812311657. CrossRef - Extravasation of monoclonal antibodies commonly used in oncology: Classification, management and the role of the pharmacist
Tiene Bauters, Nele Clottens, María A Albert-Marí
Journal of Oncology Pharmacy Practice.2023; : 107815522311786. CrossRef - Extravasation of Noncytotoxic Agents: Skin Injury and Risk Classification
Yuuka Shibata, Takanori Taogoshi, Hiroaki Matsuo
Biological and Pharmaceutical Bulletin.2023; 46(6): 746. CrossRef - Radiopharmaceutical extravasation in bone scintigraphy: a cross-sectional study
Davide Fernandes, Márcia Santos, Miguel Pinheiro, Hugo Duarte, Filipa Fontes
Nuclear Medicine Communications.2023; 44(10): 870. CrossRef - Compartment Syndrome Secondary to Calcium Gluconate Extravasation
Derek S Weimer, Sydney Jones, Tanya Ramadoss, Una Milovanovic, Mohammadali M Shoja, Gary Schwartz
Cureus.2023;[Epub] CrossRef - Profiles and Outcomes of Skin Injuries Caused by Injectable Drug Extravasation
Mika Maezawa, Misaki Inoue, Riko Satake, Wataru Wakabayashi, Keita Oura, Koumi Miyasaka, Sakiko Hirofuji, Fumiya Goto, Mari Iwata, Takaaki Suzuki, Hideyuki Tanaka, Megumi Horibe, Satoshi Nakao, Toshikazu Tsuji, Ichiro Ieiri, Kazuhiro Iguchi, Mitsuhiro Nak
Journal of Infusion Nursing.2023; 46(5): 281. CrossRef - Tissue Necrosis Following Extravasation of Human Immunoglobulin in an Infant
Yu Jing, Wanyu Jia, Peng Li, Chunlan Song
Clinical Pediatrics.2023;[Epub] CrossRef - Extravasation of Non-Cytotoxic Drugs in Older People
T’yanna Montague, Salome Bwayo Weaver, La’Marcus T. Wingate
The Senior Care Pharmacist.2023; 38(11): 457. CrossRef - A temperature-responsive intravenous needle that irreversibly softens on insertion
Karen-Christian Agno, Keungmo Yang, Sang-Hyuk Byun, Subin Oh, Simok Lee, Heesoo Kim, Kyurae Kim, Sungwoo Cho, Won-Il Jeong, Jae-Woong Jeong
Nature Biomedical Engineering.2023;[Epub] CrossRef - Effect of Pharmacoprophylaxis on Postoperative Outcomes in Adult Elective Colorectal Surgery: A Multi-Center Retrospective Cohort Study within an Enhanced Recovery after Surgery Framework
William Olin Blair, Mary Allison Ellis, Maria Fada, Austin Allen Wiggins, Rachel C. Wolfe, Gourang P. Patel, Kara K. Brockhaus, Molly Droege, Laura M. Ebbitt, Brian Kramer, Eric Likar, Kerilyn Petrucci, Sapna Shah, Jerusha Taylor, Paula Bingham, Samuel Kr
Healthcare.2023; 11(23): 3060. CrossRef - Progress in Research on the Mechanisms and Interventions of Phlebitis from the Perspective of Vascular Endothelial Cell and Signaling Pathway
Ling-Ling Zhu, Yan-hong Wang, Quan Zhou
Journal of Inflammation Research.2023; Volume 16: 6469. CrossRef - Cutaneous Management after Extravasation of High-Concentrated Amino Acid Solution Administered for Renal Protection in PRRT
Chaninart Sakulpisuti, Wichana Chamroonrat, Supatporn Tepmongkol
Tomography.2022; 8(1): 356. CrossRef - SOP Einteilung und Therapie von Paravasaten
Svenja Wulf
Onkologie up2date.2022; 4(02): 116. CrossRef - Effectiveness of structured teaching programme on knowledge regarding management of extravasation of chemotherapeutic drugs
Prakash Pooja, Chandra Ayush , Kotha Malathi , Das Santosh Kumar , Prakash Barsha , Chandra Avinash , Sherpa Gyaljin , Acharya Sudikshya
Insights on the Depression and Anxiety.2022; 6(1): 018. CrossRef - Intervenção de enfermagem perante o extravasamento de citostáticos - um contributo na prevenção da queimadura química
Ana Marcelino, Marta Ganhão
Onco.News.2022; (45): e067. CrossRef - Yenidoğan yoğun bakım ünitesinde çalışan sağlık personelinin ekstravazasyon bilgi birikimi ve yönetimi
Ayşen ORMAN, Yalçın ÇELİK, Nihan ÖZEL ERÇEL
Mersin Üniversitesi Sağlık Bilimleri Dergisi.2022; 15(3): 465. CrossRef - SOP Einteilung und Therapie von Paravasaten
Svenja Wulf
Frauenheilkunde up2date.2021; 15(02): 107. CrossRef - Tissue distribution of epirubicin after severe extravasation in humans
Jakob Nedomansky, Werner Haslik, Ursula Pluschnig, Christoph Kornauth, Christine Deutschmann, Stefan Hacker, Günther G. Steger, Rupert Bartsch, Robert M. Mader
Cancer Chemotherapy and Pharmacology.2021; 88(2): 203. CrossRef - Novel Conformal Skin Patch with Embedded Thin-Film Electrodes for Early Detection of Extravasation
Ruiqi Lim, Ramona B. Damalerio, Choon Looi Bong, Swee Kim Tan, Ming-Yuan Cheng
Sensors.2021; 21(10): 3429. CrossRef - Efficacy of combination of localized closure, ethacridine lactate dressing, and phototherapy in treatment of severe extravasation injuries: A case series
Yan-Xu Lu, Ying Wu, Peng-Fei Liang, Rong-Chan Wu, Ling-Yun Tian, Hui-Ying Mo
World Journal of Clinical Cases.2021; 9(18): 4599. CrossRef - Modern approaches for long-term venous access in oncology
Yu.V. Buydenok
Onkologiya. Zhurnal imeni P.A.Gertsena.2021; 10(3): 69. CrossRef - Elaboration and validation of an algorithm for treating peripheral intravenous infiltration and extravasation in children
Luciano Marques dos Santos, Katharinne de Jesus Nunes, Cleonara Sousa Gomes e Silva, Denise Miyuki Kusahara, Elisa da Conceição Rodrigues, Ariane Ferreira Machado Avelar
Revista Latino-Americana de Enfermagem.2021;[Epub] CrossRef - Measuring the Validity and Reliability of the Vascular Access Complication Staging and Treatment Instrument in a Pediatric Population
Genieveve J. Cline, Virginia Pohlod, Kristina J. Burger, Ernest K. Amankwah
Journal of Infusion Nursing.2021; 44(4): 225. CrossRef - Chemotherapy Extravasation: Incidence of and Factors Associated With Events in a Community Cancer Center
Nancy Ehmke
Clinical Journal of Oncology Nursing.2021; 25(6): 680. CrossRef - Drug Extravasation in a Large General Hospital in Hunan, China: A Retrospective Survey
Zhihong Gong, Jinghui Zhang, Jianmei Hou, Shujie Chen, Zixin Hu, Xiaoya Kong, Guiyuan Ma, Lingxia Luo
Risk Management and Healthcare Policy.2021; Volume 14: 4931. CrossRef - The Journal Citation Indicator has arrived for Emerging Sources Citation Index journals, including the Journal of Educational Evaluation for Health Professions, in June 2021
Sun Huh
Journal of Educational Evaluation for Health Professions.2021; 18: 20. CrossRef

 KHPLEI
KHPLEI

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


