Educational strategies for teaching evidence-based practice to undergraduate health students: systematic review
Article information
Abstract
Purpose
The aim of this systematic review was to find best teaching strategies for teaching evidence-based practice (EBP) to undergraduate health students that have been adopted over the last years in healthcare institutions worldwide.
Methods
The authors carried out a systematic, comprehensive bibliographic search using Medline database for the years 2005 to March 2015 (updated in March 2016). Search terms used were chosen from the USNLM Institutes of Health list of MeSH (Medical Subject Headings) and free text key terms were used as well. Selected articles were measured based on the inclusion criteria of this study and initially compared in terms of titles or abstracts. Finally, articles relevant to the subject of this review were retrieved in full text. Critical appraisal was done to determine the effects of strategy of teaching evidence-based medicine (EBM).
Results
Twenty articles were included in the review. The majority of the studies sampled medical students (n=13) and only few conducted among nursing (n=2), pharmacy (n=2), physiotherapy/therapy (n=1), dentistry (n=1), or mixed disciplines (n=1) students. Studies evaluated a variety of educational interventions of varying duration, frequency and format (lectures, tutorials, workshops, conferences, journal clubs, and online sessions), or combination of these to teach EBP. We categorized interventions into single interventions covering a workshop, conference, lecture, journal club, or e-learning and multifaceted interventions where a combination of strategies had been assessed. Seven studies reported an overall increase to all EBP domains indicating a higher EBP competence and two studies focused on the searching databases skill.
Conclusion
Followings were deduced from above analysis: multifaceted approach may be best suited when teaching EBM to health students; the use of technology to promote EBP through mobile devices, simulation, and the web is on the rise; and the duration of the interventions varying form some hours to even months was not related to the students’ EBP competence.
Introduction
Evidence-based practice (EBP) has been defined as the ‘interpretation of the best research evidence with clinical expertise and the patient’s unique values and circumstances’ [1]. It is an approach to clinical decision-making that has gained considerable interest over recent years within the healthcare field [2]. It is important that higher institutions always strive for the most effective approach to teaching students the knowledge and skills required for EBP, so that upon commencing clinical practice they can confidently incorporate research evidence into their clinical decision-making. This systematic review brought together the existing teaching strategies for EBP that have been adopted over the last years in healthcare institutions worldwide. The specific objective of this review was to identify best teaching strategy for teaching EBP to undergraduate health students. Also, recent trends of EBP were deduced.
Methods
Literature search strategy
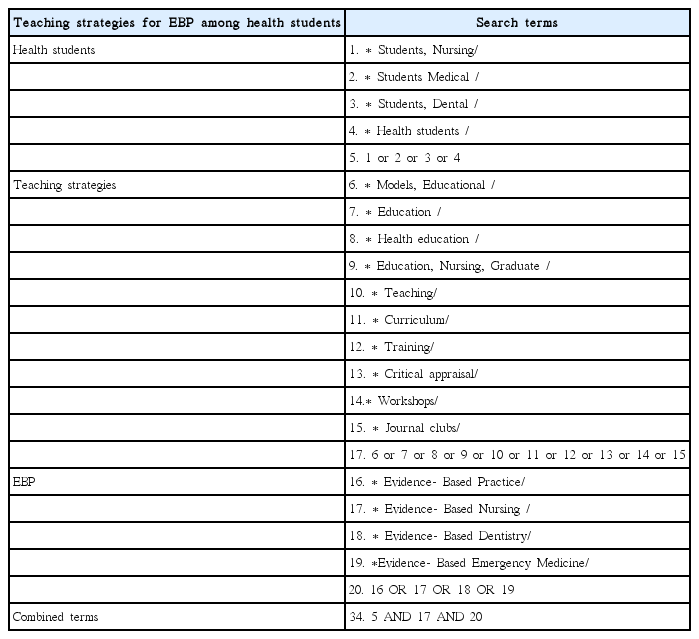
A systematic review of the existing literature on the existing strategies to teach EBP to undergraduate health students was carried out. We posed the following review question: “What are the existing strategies appropriate for teaching EBP to undergraduate health students?” We drew up a review protocol in advance following standards outlined in the MOOSE (Meta-analysis of Observational Studies in Epidemiology) guidelines for meta-analyses and systematic reviews of observational studies [3]. Next we carried out a systematic, comprehensive bibliographic search using Medline database for the years 2005 to March 2015 (updated in March 2016). Search terms used were chosen from the list of MeSH (Medical Subject Headings) and free text key terms were used as well. The search algorithm used was: (“Students, Nursing” OR “Students Medical” OR “Students, Dental” OR “Health students”) AND (“Models, Educational” OR “Education” OR “Health education” OR “Education, Nursing, Graduate” OR “Teaching”; “Curriculum” OR “Training” OR “Critical appraisal” OR “Workshops” OR “Journal clubs” OR “Evidence-Based Practice” OR “Evidence-Based Nursing” OR “Evidence-Based Dentistry” OR “Evidence-Based Emergency Medicine”). Full details of the search strategy and the keywords’ combination are provided in Table 1. The same search method was then repeated using the EMBASE database. Bibliographies of each retrieved study and reviews were also checked by hand for additional studies that met broad eligibility criteria.
Selection criteria
From the identified papers, studies meeting the following eligibility criteria were selected: (1) Papers published in peer-reviewed journal as high quality literature was of interest; (2) Papers published in English language as authors had not advanced skills of other languages; (3) Papers published during the last 10 years as up-to-date knowledge was considered necessary; (4) Study designs including randomized controlled trials, controlled trials or cohort studies (pre-post longitudinal studies); (5) Studies that focused on educational interventions (no restrictions placed upon the mode of delivery or the type) to increase EBP competence among undergraduate health students; (6) Studies that evaluated EBP outcomes pre- and post- the educational intervention irrespective of the presence of comparator groups; (7) Studies that performed quantitative estimates of the effectiveness of EBP educational approaches on the outcome of interest (EBP related competence, knowledge, attitudes, skills).
Studies not meeting these criteria were excluded and studies meeting the criteria were shortlisted for inclusion in the review.
Literature screening and data extraction
Studies were evaluated for inclusion by two independent reviewers for relevance to the subject. Study selection was accomplished through three levels of study screening. At level 1 screening, studies were excluded by reviewing the title of the article. At level 2 screening, abstracts of all studies accepted at level 1 were reviewed for relevance. For level 3 screening, the full text was obtained for relevant papers and any citations for which a decision could not be made from the abstract. Where there was uncertainty, discussion was held with the research team to reach consensus. Information on study design, methods and outcomes were obtained by using a previously piloted data extraction form. The following information was extracted verbatim from each included study: research design, health student discipline, sample size, EBP intervention, instrument used, effect sizes, and key message.
Results
Bibliographic search
Our combined search to MEDLINE and EMBASE retrieved 973 records. The initial screening of manuscript titles and abstracts excluded 799 records. We excluded another 155 articles after examination of the full text. Additionally, two articles were retrieved by searching the reference lists of the retrieved reviews and articles. Fig. 1 shows the numbers of studies identified and selected/excluded in each phase of the search. Ultimately, 20 articles were deemed suitable for inclusion in the review.
Studies’ characteristics
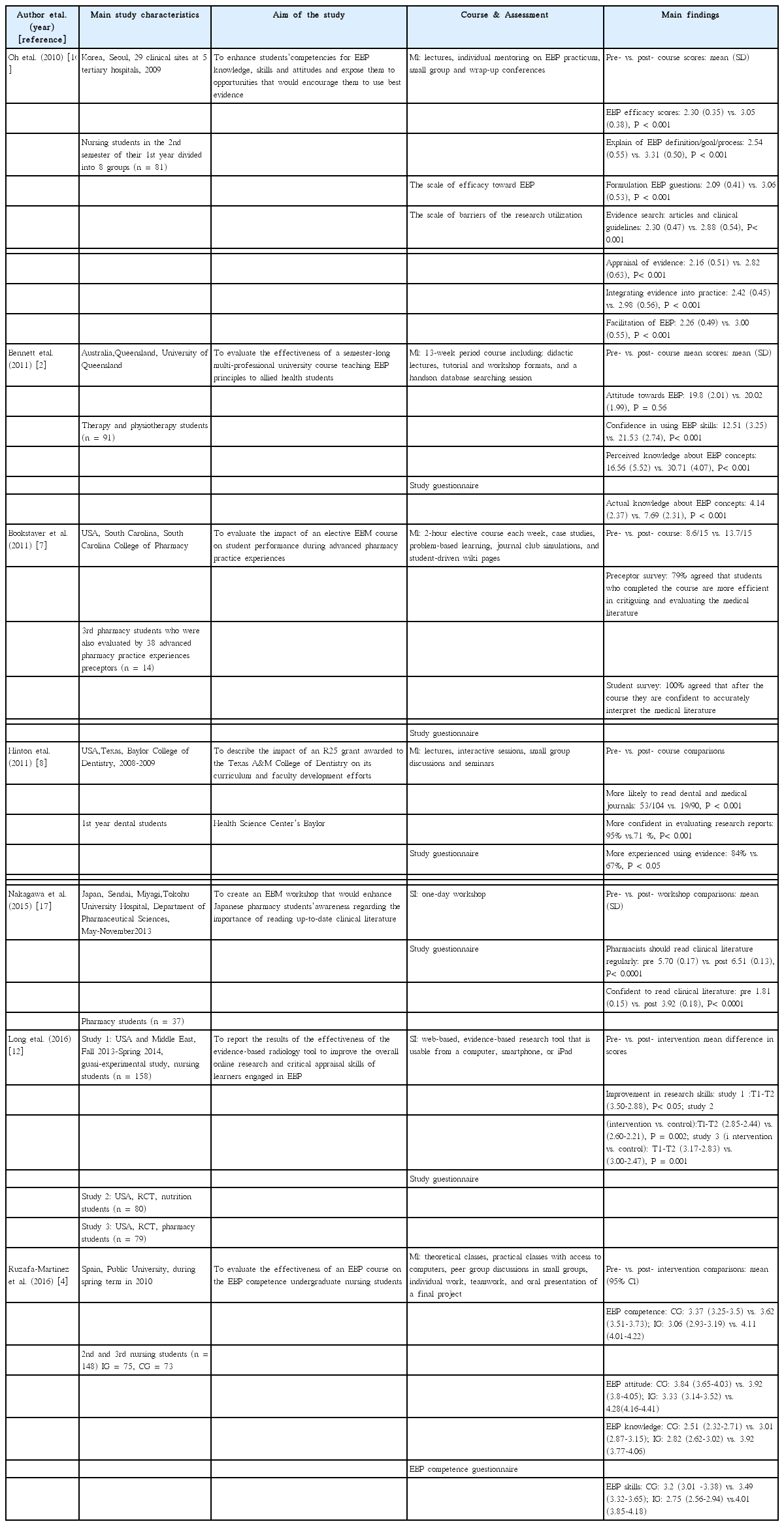
One study was conducted in a European country, Spain [4], and nineteen studies in non-European countries including US [5-12], Mexico [13,14], Australia [2,15], Korea [16], Japan [17], Malaysia [18], Thailand [19], Taiwan [20], Jordan [21], and Nigeria [22]. Seventeen studies have been published since 2010 [2,4,6-18,20,21]. Of the 20 studies, 16 were pre-post (uncontrolled) studies and four were controlled trials [4,5,12,15]. Controlled studies compared the intervention group to a control group with no intervention. The sample size for the included studies ranged from 14 to 319 students. The majority of studies sampled medical students (n=13) [5,6,9-11,13-15, 18-22] and the remaining studies nursing (n=2) [4,16], pharmacy (n=2) [7,17], physiotherapy/therapy (n=1) [2], dentistry (n=1) [8] students, or students from mixed disciplines (n=1) [12]. Studies evaluated many different educational interventions of varying duration, frequency and format (lectures, tutorials, workshops, conferences, journal clubs, and online sessions), or combination of these to teach EBP. We categorized interventions into single interventions (SI) covering a workshop, conference, lecture, journal club, or e-learning [2,4,5,7,8,10,12,14-17,19,20,22] and multifaceted interventions (MI) where a combination of strategies had been assessed [6,9,11,13,18,21]. Similarly, the duration of training ranged widely, from 2 hours to 1 year. Interventions covered different steps of the EBP domains (research question, sources of evidence, evidence appraisal, and implementation into practice). All but seven studies reported using valid and reliable instruments [4,6,9,14,16,21]. Two studies used the Fresno test [6,21], one the Fresno test and Berlin questionnaire [9], one the Taylor questionnaire [14], one the Scale of efficacy toward EBP [16], one the EBP competence questionnaire [4], and one a validated instrument for assessment of EBP related knowledge [20]. Knowledge, attitudes, and EBP skills were the outcomes most commonly explored among the included studies. The majority of the studies assessed the effect of the intervention soon after the delivery of the intervention and only 2 studies examined the longer term effect, one 2 months [4] and one 6 months [15] following the intervention. A detailed presentation of the characteristics of the studies and included interventions is provided in Table 2 and Table 3.

Summary of studies conducted among medical students on teaching strategies for evidence-based practice among health students
Synthesis of results
Due to the heterogeneity of interventions used and outcomes measured across studies a meta-analysis was not performed. A narrative synthesis of the key-findings of the studies included in the review will be presented below.
Seven studies reported an overall increase to all EBP domains indicating a higher EBP competence and 2 studies focused on the searching databases skill. Liabsuetrakul et al. [19] in 2009 offered a SI (small group sessions) to medical students. In this study 3 assessments were performed, before, in the middle and after the EBM course and findings showed that the students’ skills in the middle and after the course were improved significantly compared to ratings before the delivery of the course [19]. The second study offered a SI (two sessions, one provided in the middle and the other at the end of the semester) to nursing students [16]. Before the intervention, the overall and individual subscale scores for EBP efficacy had an overall mean score of 2.30, indicating that the students were ‘a little confident.’ After the intervention, the scores increased to a mean of 3.05, indicating that students felt ‘confident’ regarding the EBP process.
West et al. [9] organized a MI, which included didactic, small-group sessions and EBP assignments, for 2nd year medical students. EBM knowledge scores on the 15-point Berlin questionnaire increased from baseline by 3.0 points at the end of the second year of the course and by 3.4 points at the end of the third year (P<0.001). EBM knowledge scores on the 212-point Fresno test increased from baseline by 39.7 points at the end of the course and by 54.6 points at the end of the third year (P<0.001). Barghouti et al. [21] assessed the effectiveness of MI (lectures, seminars, online search, and answering worksheets) offered to medical students. The students were asked to complete the Fresno test pre- and posttest and findings showed that the mean difference between the pre- and posttests was 92.8 (P<0.001).
A quasi-experimental study conducted in Spain among nursing students included MI i (lectures, practicals, group discussions, teamwork, and students’ presentations) designed to teach EBP competence [4]. The EBP competence questionnaire was administered before and at two months after the 15-week intervention period and results showed that the mean scores of the intervention group were significantly improved versus baseline in skills (4.01 vs. 2.75) dimensions. Another study conducted in Japan among pharmacy students was designed as one-day MI (students’ presentations, lectures, and small group discussions) and findings showed a significant improvement in the overall scores on the EBM test: 11.4 (0.29) vs. 12.6 (0.22), P<0.0001) [17].
The latest study was conducted by Long et al. [12] and tested a web-based EBP tool that is usable from a computer, smartphone, or iPad. Findings showed that a significant improvement in overall research skills among the nursing and nutrition student group.
Two interventions offered to medical students were found to increase the ability of students in performing effective literature searches [5,18]. The first study designed by Gruppen et al. [5] aimed to quantify the impact of a SI (two-hour) intervention on techniques for searching Medline for evidence related to a clinical problem. Findings showed that the intervention students had fewer search errors and correspondingly higher quality searches than did the control students. The second study involved final-year medical students who received MI (lectures and small-group clinical sessions) and findings showed that students who searched PubMed or Medline for more than three times per week increased from 9.7% to 31.7% (P<0.001) [18].
Six studies examined the effect of an intervention on students’ EBP knowledge and attitude. Two of them have been previously described [4,19]. Ruzafa-Martinez et al. [4] showed that attitudes and knowledge scores were significantly improved versus baseline after the EBP course (4.28 vs. 3.33 and 3.92 vs. 2.82, respectively) [9]. Similarly, Liabsuetrakul et al. [19] showed significantly higher scores for attitude over time following the intervention (P<0.001). Okoromah et al. [22] delivered a SI (3 month course) offered to medical students from Nigeria. A statistically significant increase in students’ self-reported knowledge and attitudes regarding EBM was found. Mean scores for their understanding of the EBM concepts increased from 2.20 (0.85) to 3.17 (0.80) on a 4-point rating scale (P<0.001). Another study included occupational therapy and physiotherapy students who completed MI (lectures, tutorial and workshop formats, and database searching session) over a 13-week period (2 hours per week). Following the MI students’ perceived knowledge improved with a statistically significant mean increase of 14.15 (score range, 5 to 25; 95% confidence interval [CI], 12.55 to 15.75) and there was a statistically significant mean increase in actual knowledge of 3.56 (score range, 0 to 10; 95% CI, 2.83 to 4.29) [2]. West et al. [9] offered MI (‘short course’ with didactic, small-group sessions and EBP assignments) to medical students. On a 5-point scale, self-rated EBP knowledge increased from baseline by 1.0 and 1.4 points, respectively (both P<0.001). A year later another study was published by Cheng et al. [20] in 2012. Authors offered either a weekly EBP-structured case conference or a weekly didactic lecture about EBP to final year medical students. The teaching effects of these 2 interventions were evaluated by a validated instrument for assessment of EBP related knowledge. When compared to students in the didactic lecture group, students in the EBP conference group had significantly higher post-intervention scores of EBP knowledge: 21.2 (3.5) vs. 19.0 (4.6), P<0.01.
Discussion
On the whole, EBP teaching to future healthcare professionals has mainly been documented in medical students. Many different educational interventions of varying duration, frequency, and forma to teach EBP in a variety of settings exist. It showed that educational strategies adopted were found to improve students’ overall EBP competence and their EBP knowledge and skills. Students felt more confident to accurately interpret the literature, could better assess the reliability/validity of information on the web and felt more comfortable with the concepts of EBP.
It indicated that EBP is a learnable skill and the question is not whether EBP can or should be taught, but how to best teach [23]. The challenge for nursing academics is to find innovative ways to engage students in a way that facilitates the development of positive attitudes to research so that knowledge utilization and translation are skills all future nurses and health professionals actively use. However, there is little robust evidence to guide the most effective way to build EBP knowledge and skills in undergraduate health students. Towards this direction, the first question to be answered is when EBP teaching should be first introduced into the curriculum. Our findings provide us with inconclusive evidence regarding the best possible time for EBP introduction to the health curriculum. Burns and Foley [24] in 2005 supported EBP inclusion in the first year aiming to foster an EBP approach to clinical practice, but others supported its introduction at a later stage after training in research methods [25]. This is in line with other researchers who support the need for students to learn basic epidemiology and statistics before taking a specific EBP course, which is facilitated by statistical knowledge and contextualizes it in a critical framework, investing it with greater meaning and relevance for the students [26].
The second critical question is how EBP should be taught in order to increase students’ engagement and foster students’ learning experience. Our review showed that existing studies have used different approaches including didactic lectures, computer sessions, group discussions, class activities, or a combination of these. Existing evidence supports, however, the idea that MI have been demonstrated more likely to improve knowledge, skills, and attitudes compared to SI offered over a short duration or to no interventions [4,27]. MI, with combinations of methods including lectures, computer sessions, small group discussions, journal clubs, and assignments were more likely to improve knowledge, skills, and attitude compared to SI or no interventions. As a result, a multifaceted approach may be best suited when teaching EBM to health students.
Furthermore, the use of technology to promote EBP through mobile devices, simulation, and the web is on the rise and web-based educational platforms have been demonstrated as an effective and desirable mechanism to deliver educational content to health professionals [28,29]. Our review showed that the use of online material and tools to teaching EBP is in its infancy as only 2 studies adopted an online approach to teach EBP and concluded that the use of technology to teach research skills can facilitate EBP teaching [6,12]. Future studies should take advantage of the technology improvements and achievements and incorporate the use of internet and widely used smartphone applications with the aim to foster online interactive learning and engagement [30].
In addition, the duration of the interventions varying form some hours to even months was not related to the students’ EBP competence. An important aspect that should be considered in future research is the frequency of the delivery of the intervention as continuous or repeated interventions may help more so that not only do students become more comfortable with EBP, but also they remain comfortable for a longer period of time. As in the majority of the studies the pre- and post-test duration was too short that may lead to recall bias, meaning that we need further evaluation of the course to determine its effect on the students after a longer period. Better methodologies for identifying EBP competencies retention in the long term should be undertaken.
Finally, validated tools to assess knowledge and skill acquisition exist and have been widely used but similar, validated tools to determine the extent to which attitudes change after an educational intervention are lacking [31]. Most studies reporting change in attitude or behaviour rely on student self-reports as measurements tools, but this is not reliable method for measuring long-term changes in attitude [31]. In addition, increase in EBP competency is dependent on a variety of factors including prior training and exposure to epidemiology, research design, biostatistics, and organizational culture and support toward EBP. None of the studies identified in this review adjusted for these potential confounding factors. Therefore, it is difficult to estimate what effect, if any, these factors contribute to participants’ EBP competency across undergraduate and post-graduate settings.
A limitation of this systematic review is the fact that due to the heterogeneity of interventions used and outcomes measured across studies a meta-analysis was not performed. More comprehensive studies are needed to resolve many important issues concerning the effective methods to teach EBP among health students. Specifically, further studies are required to clarify issues as to when, how and by whom EBP should be taught. In addition, future research should examine the effectiveness of use of technology improvements and online communication tools on fostering online interactive learning and engagement. In addition, future studies need to adopt better methodologies and validated tools for identifying EBP competencies retention in the long term and for determining the extent to which attitudes change following the implementation of an educational intervention.
In conclusion, above results told us that multifaceted approach may be best suited when teaching EBM to health students. The use of technology to promote EBP through mobile devices, simulation, and the web is on the rise. Also, the duration of the interventions varying form some hours to even months was not related to the students’ EBP competence.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Supplementary materials
Audio recording of abstract.