How prepared are medical students to diagnose and manage common ocular conditions
Article information
Abstract
It is essential that primary care physicians have a solid fund of knowledge of the diagnosis and management of common eye conditions as well as ocular emergencies, as management of these diseases commonly involves appropriate referral to an ophthalmologist. Thus, it is crucial to receive comprehensive clinical knowledge of ophthalmic disease in the primary care setting during medical school. This study investigated how well prepared medical students are to diagnose and manage common ocular conditions. The study used scores from a standardized 12-question quiz administered to fourth-year medical students (N = 97; 88% response rate) and second-year medical students (N = 97; 97% response rate). The quiz comprising diagnosis and referral management questions covered the most frequently tested ophthalmology topics on board exams and assessed students’ ability to recognize when referral to an ophthalmologist is appropriate. Fourth-year medical students had quiz scores ranging from 0%-94.5% with an average score of 68.7%. Second-year students had quiz scores ranging from 27.2%–86.4%, with an average score of 63.8%. Passing rate was 70%. Student’s t-test showed fourth-year students had a significantly higher quiz average (P = 0.003). In general, both classes performed better on diagnostic questions (fourth-year, 73.7%; second year, 65.8%) rather than on management questions (fourth-year, 64.8%; second year, 61.8%). Both second-year and fourth-year students on average fell short on passing the ophthalmology proficiency quiz, and in general students were more adept at diagnosing rather than managing ocular conditions and emergencies.
Since 2000, the number of medical schools requiring an ophthalmology rotation has declined from 68% to 30% in 2004 [1]. The Liaison Committee on Medical Education does not require training in this subspecialty during medical school. Thus, academic policies have led to lack of financial support for ophthalmology teaching and equipment, driving academic departments away from medical school involvement. Although there have not been formal studies to assess the consequence of a lower prevalence of ophthalmology in medical school curricula, there have been editorial observations suggesting that primary care residents are inadequately trained to deal with initial management or appropriate referral of basic ophthalmic diseases [1]. Despite the decline in medical school education, primary care residencies expect their incoming residents to have solid ophthalmology exam skills and knowledge. The Association of University Professors of Ophthalmology (AUPO) has recommended that all graduating medical students be able to: measure and record visual acuity, evaluate a red eye, evaluate a traumatized eye, detect strabismus, detect pupillary abnormalities, perform direct ophthalmoscopy and initiate appropriate management and referral for common ocular conditions. The AUPO surveyed 135 primary care residencies, including Family Medicine, Internal Medicine, and Pediatrics. Ninety percent of program directors believe that the greater than 50% of their entering residents meet the AUPO standard. Moreover, 85% of program directors believe a major component of ophthalmology training should occur during medical school. While ophthalmology expertise was assessed in 92% of Family Medicine programs, less than 30% of Internal Medicine and Pediatric residencies did so. There is a deepseated disconnect between residency program expectations and prioritization of ophthalmology education in medical schools. Currently, the ophthalmology curriculum at the medical school where this study was conducted is concentrated within the first two years of medical education. During the first year, students are taught how to use an ophthalmoscope and locate the optic nerve on exam. During the second year, students are given a lecture covering the signs and symptoms the most common eye conditions. The medical school does not have a required ophthalmology lecture during the third-year surgery clerkship, nor a required fourth-year ophthalmology elective. Thus, the purpose of this research was to investigate how well fourth-year medical students retained knowledge of how to diagnose common eye conditions and how prepared they are to recommend consultation within the primary care setting. Additionally, we investigated how well second-year medical students learned the ophthalmology curriculum, and how their testing skills compared to their senior medical students. Thus far, there have been no needs assessment studies for ophthalmology medical education in the United States.
With institutional review board approval, the study used anonymous scores from a standardized 12-question quiz with forced choice responses voluntarily administered to fourth-year medical students (N=97; 88% response rate) and second-year medical students (N = 97; 97% response rate) in large group format during class time. The quiz, comprised of diagnosis and referral management questions, covered the most frequently tested ophthalmology topics on United States Medical License Examination (USMLE) Steps 1 and 2. The quiz also assessed students’ ability to recognize when referral to an ophthalmologist was appropriate, and how urgent the referral should be (within one to two days versus within two weeks). The quiz was constructed using physicians with expertise in ophthalmology, as well as various study resources including the American Academy of Family Practice board review and the International Council of Ophthalmology medical student handbook. The quiz was pilot tested. The scores are maintained in a deidentified database that used randomized participant numbers. Statistical analysis on students’ quiz scores was conducted to determine the class’s performance on the quiz and to assess if there are certain medical topics that proved to be areas of weakness. Moreover, analysis compared students’ performance in clinical diagnosis to performance in clinical recommendations for follow up, to assess if there is weakness in this area of clinical reasoning.
Fourth-year medical students had quiz scores ranging from 0%-94.5% with an average score of 68.7%. Second-year students had quiz scores ranging from 27.2%–86.4%, with an average score of 63.8%. A passing score for the quiz was set at 70% as this is the standard passing grade for most quizzes and tests administered at the study site. Student t-test showed fourth-year students had a significantly higher quiz average (P=0.003). In general, both classes performed better on diagnostic questions (fourth-year, 73.7%; second-year, 65.8%) rather than on management questions (fourth-year, 64.8%; second-year, 61.8%). In terms of diagnosis, both second-year and fourth-year students passed on questions regarding acute angle closure glaucoma, temporal arteritis, cataract, macular degeneration, and corneal abrasion. Fourth-year students additionally passed on diagnosing conjunctivitis and subconjunctival hemorrhage, whereas second-year students did not. Both second-year and fourth-year students did not pass on questions regarding diagnosis of retinal detachment, proliferative diabetic retinopathy, and central retinal artery occlusion (Table 1). In terms of management, both second-year and fourth-year students passed on questions regarding on acute angle closure glaucoma, cataract, central retinal artery occlusion, and temporal arteritis. Fourth-year students additionally passed on retinal detachment and subconjunctival hemorrhage. On management questions, both second-year and fourth-year students on average did not pass on the following topics: macular degeneration, diabetic retinopathy, adult strabismus, pediatric strabismus, conjunctivitis, and corneal abrasion (Table 2).
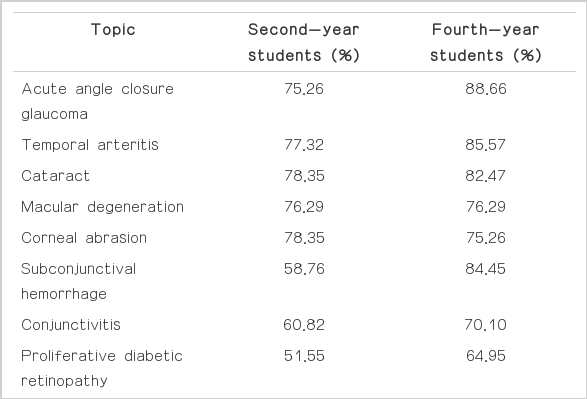
Comparison of second-year and fourth-year medical students’ performance on diagnostic questions in Wright State University Boonshoft School of Medicine, Dayton, OH, USA

Comparison of second-year and fourth-year medical students’ performance on management questions in Wright State University Boonshoft School of Medicine, Dayton, OH, USA
According to our study, there is a significant gap in knowledge with regards to diagnosis and management of common ocular conditions and ocular emergencies in fourth-year medical students, as well as in second-year medical students. Both second-year and fourth-year students on average fell short on passing the ophthalmology proficiency quiz. This is concerning as primary care residents are expected to become proficient in the timely diagnosis of common ocular conditions. In particular, both classes fell short of recognizing and managing proliferative diabetic retinopathy, which is a disease that is rapidly growing in prevalence as the number of diabetics increase and their live expectancy increases as well. Another observation is that in general students were more adept at diagnosing rather than managing ocular conditions and emergencies. Perhaps there should be more of an emphasis in our curriculum regarding referral management; the current emphasis in our curriculum is on pattern recognition of disease and its presenting signs and symptoms. Both second-year and fourth-year students were more comfortable in diagnosing anterior segment questions rather than posterior segment questions, i.e., retinal detachment, proliferative diabetic retinopathy, and central retinal artery occlusion. Perhaps this demonstrates a weakness in our school’s curriculum, and more education should thus be concentrated on posterior globe topics. It may also demonstrate that these topics may be more difficult to master in medical school. Moreover, it may show that anterior segment questions had more “buzzwords” or pattern recognition adjectives that students may have recognized from their board review questions. Interestingly, although students may not have performed well on diagnosis of retinal detachment or central retinal artery occlusion, they choose the correct management. This demonstrates good clinical judgment that is consistent from second-year students to fourth-year medical students. As a resident and practicing physician in the fields of Internal Medicine, Family Medicine, Pediatrics, and Emergency Medicine, it is essential to have a solid fund of knowledge regarding common ocular conditions. Several critical eye conditions require referral to an ophthalmologist within a matter of hours to days from the onset of symptoms. Typically patients will present as an urgent visit to their primary care physician or to the emergency room in these situations. Thus, it is crucial to receive a strong foundation in the diagnosis and management of common ophthalmic diseases while in medical school. This study highlights the need for integration of ophthalmology education within all four years of medical school and the necessity of greater emphasis on referral management during clinical training.
Notes
No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIAL
Audio recording of the abstract.